Patient notes are important in the medical field. The purpose of these notes is to record the health status and condition of the patient over time while he is being treated in a hospital.
This report helps medical practitioners see the achievements of the patient in recovering from a particular health problem. There are some systematic and organized methods through which the progress is reviewed and noted.
The doctor then uses this progress note to make any necessary decisions regarding the health of the patient. For example, whether the patient should be discharged from the hospital is decided based on the progress report.
The objective of making progress notes in many hospitals is to ensure that the patient is being given the best health care. The type and format of the progress notes depend on the information to be added to them and the hospital that is making these notes.
Why do we need patient progress notes?
Patient progress notes are needed to check if the patient is showing progress. Hospitals that are required to make some important decisions about the patient should read these notes. For example, if a surgeon is going to conduct surgery, he should read the progress notes to learn about his health in detail.
Patient progress notes as an MS Word document
In general, the patient progress notes are prepared in MS Word document. These notes do not require any calculation to be performed. Therefore, MS Word is a suitable file format to be used. It is easy to edit these notes in MS Word. Moreover, notes prepared in MS Word are easy to print.
How do I write progress notes?
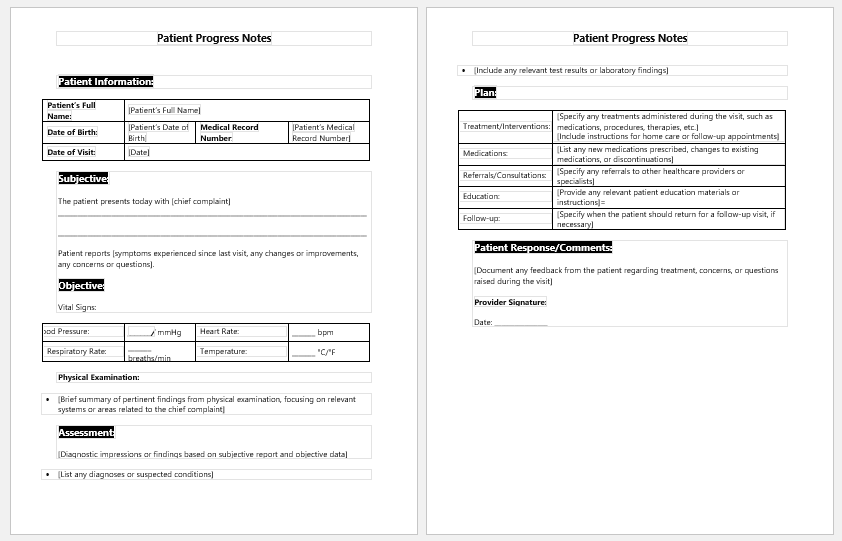
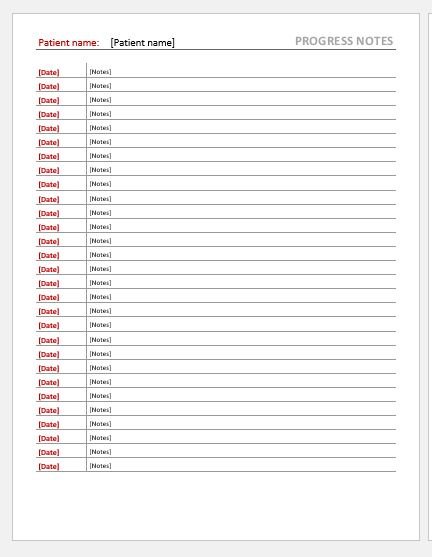
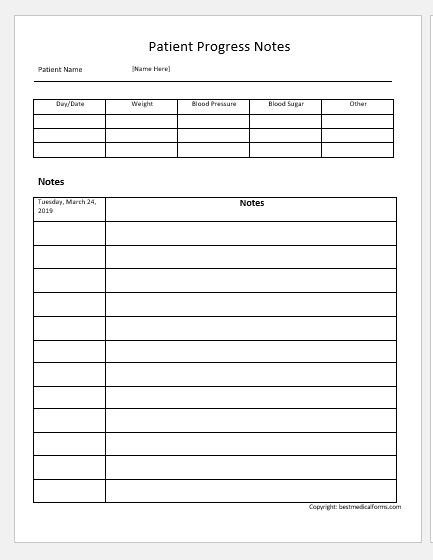
You need to know how to write progress notes. The patient progress notes are not too long; rather, they are brief and to the point. The focus while writing progress notes should be on the development of the patient during the specific period. This can be written by comparing the previous progress notes with the current condition.
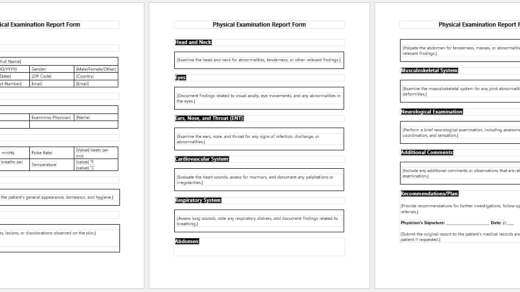
Different details are added to the progress notes. These notes include information about the patient, such as name, patient ID, room or bed number, etc. The lab findings and other test results are mentioned in the notes.
The diagnosis details of the patient should also be written in these notes. You should comment on the diagnosis to let the reader know if the diagnosis is improving or not. The number of problems with the patient should be discussed.
It should be kept in mind that the notes should not be too long. You can summarize the details to make it easier for you to describe everything briefly without removing any important details. The notes should be divided into sections so that different details can be distinguished. It should be noted that patient progress notes should comprise one page at most.
Internal medicine progress note
Internal medicine progress notes are prepared to see the effects of medicine on the patient. When a doctor treats a patient, he prescribes different types of medicines. It is important to see how medicine is affecting the patient.
Based on these notes, the doctor can continue or discontinue the medicine. Internal medicine progress notes should tell for how long the patient has been taking the medicine, the effects of the medicine on the patient, the improvement seen in the patient, and a lot more.
Patient progress note templates
The patient progress notes template is available in MS Word format. This template is a powerful tool and helps hospital management in every possible way.
If the user finds this template insufficient because it lacks several details, he can easily add details to this document through its customization feature. You can easily download and save it on your PC for later use.
Preview
Preview
- Medical Expense Reimbursement Claim Form
- Patient Enrollment Form Template
- TB Assessment Form for Employment
- Low-Carb Food Shopping List
- Emergency Prep Kit Checklist
- School Immunization Record Sheet
- Home Health Care Log
- New Patient Intake Sheet
- Discontinued Medication Tracker
- Restylane Consent Form
- Dental Assessment Form
- Nutrition Assessment Form
- Clinical Consent Form
- Physiotherapy Consent Form
- Fibromyalgia Journal