Weight is an important parameter in any physical examination. It helps in the assessment of the health of patients in any age group. We all agree that there is always a certain limit to normal weight for specific ages and heights.
Excessive weight puts a man at risk of serious illnesses and health issues. Similarly, low weight or being underweight is an indication of underlying diseases and points towards low possible immunity.
For these reasons, weight assessment is very important and is done very carefully, especially in children and adults suffering from some chronic illness like AIDS, cancer, etc.
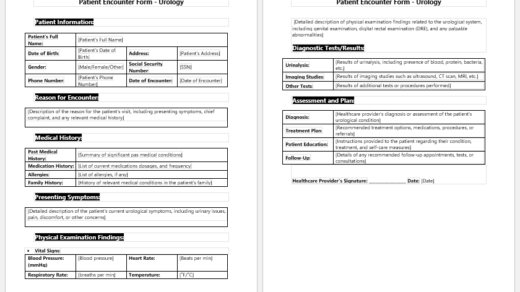
How is a patient’s weight assessment form filled out?
- A patient’s weight assessment form is filled out in a very meticulous manner, and the physician who is filling out the form needs to know the background history of the patient for the purpose.
- The identity of the patient in the initial columns is filled with care, including his name, age, gender, date of birth, contact number for follow-up, height, and current weight.
- It will be a plus if we get to know the race of the patient, which helps in assessing what the normal height and weight are for that particular race.
- The medical history of such patients is important to note down since it gives us strong evidence of the reasons why this patient is gaining or losing weight. Medical history includes any known medical illness like hypertension, diabetes, hyper or hypothyroidism, cancer, allergies, drug history, and history of any surgeries or injuries in the past.
- Besides knowing the medical history of the patient, we are interested in knowing the family history of this patient too. Any medical history of diabetes, raised blood pressure, cancer, or AIDS is inquired about. We also want to know if any of the family members died of or have suffered from a stroke, paralysis, depression, bipolar disorder, headaches, sleep disorders, or any other important illness.
- The patient is asked about filling out a little questionnaire. His self-assessment also inquired about how he feels about his health. He is asked about any history of depression, smoking, obsessive habits, or alcoholism. If he is a smoker, his frequency of smoking is mentioned, as is alcoholism.
- He also inquired about how often he eats fast food. His sleeping habits, dietary habits, and relationships with colleagues and family members are required. He has to mention if he is currently on any medication.
- Knowing the nutritional status of the patient is very important. His dietary habits affect mostly his weight, and they help to reach the cause of being abnormally overweight or underweight. We do want to know how much he eats per serving or per meal, how much he drinks, what kind of food is mostly in his routine diet, and if he is in the habit of drinking coffee or tea.
- His exercise status is also asked at the end of the form, as is his birth history. Their birth weight and condition at that time and in childhood also give us a great idea of why he is suffering from his current weight.

Assessment Form File: 41 KB
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Patient Registration Confirmation Messages
- Quotation Letter for Medical Services
- Mental Health Letter by Doctor
- Excuse Letter for Absence due to Medical Checkup
- Response Letter to Feedback on Improvement in Hospital
- Letter to a Mother Who Miscarried
- Patient Feedback Letter Complaining on Issues or Incidents
- Letter to Family about Miscarriage
- Patient Constructive Feedback Letter for Quality Care Improvement
- Registered Nurse Designation Letter
- Patient Feedback Letters
- Medical Expense Reimbursement Request Letter
- Warning Letter for Immediate Improvement Required for Professional Healthcare Duties
- Excuse Letter for Stomach Pain