Examination in the medical field is one of the strongest foundations of the field. A physical examination is the first step toward better-managing patients and their ailments. Whenever a patient comes to the hospital, he comes with certain complaints. These complaints must be addressed. A technical way of addressing such problems starts with a detailed history of the patient.
An initial examination report is used to maintain a record of the patient. A patient who enters a hospital always has some significant findings that can only be detected by the initial examination conducted by the doctor. This examination is always reported and documented properly. This first-time examination carries a lot of importance and gives the foundation for a strong diagnosis and effective decision-making for the management of the patient.
Initial examination report
Let’s have a look at a general initial examination report to see how it is filled out and the important points to be mentioned in the initial report.
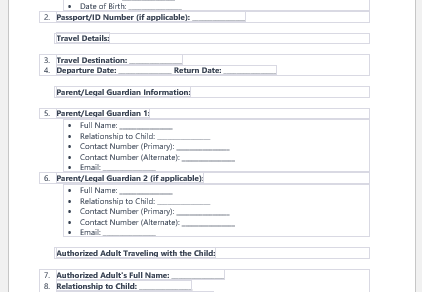
- The personal information of the patient is the most important section of any medical form. The patient’s full name, age, gender, date of birth, contact number, emergency contact number, and address—everything has to be mentioned in the information section. Not just for future reference, this information is also one of the best ways to establish the identity of the patient.
- Similarly, a doctor’s name and relevant information, along with his valid registration number, have to be mentioned.
- After that, the patient’s ailment is mentioned. The duration of the injury or illness is mentioned, and then his presenting complaints are noted down.
- If the patient has medical insurance, it is important to mention the details of his medical insurance as well. Some diseases take a lot of time, energy, and resources, which the insurance company has to bear. The hospital needs to mention that detail in its documents.
- After the general physical and systemic examination is done, the doctor may want to suggest some initial tests to help him reach a diagnosis of his problem. These tests are to be mentioned in the initial examination report.
- If the laboratory test, x-ray, or ultrasound examination has already been done, reports of these tests are also mentioned. This also helps in getting a complete idea of the problem of the patient and how he was approached by the doctor.
- The initial management or prescription of the drugs by the physician is also mentioned in this form. If the patient was given further tests, that is also mentioned in the management section of the form. Otherwise, how the patient’s management plan has to be followed must be the content of this section.
- In the end, the doctor can add some additional notes or instructions if he feels it is necessary to mention them. If the patient is going home, he may be advised about certain things in the notes section.
- The doctor then signs the document, and it is kept safe with the other records of the patient. This report can be used for future reference.
- Nursing Documentation Templates
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Pain Diary Worksheet Template
- Forms Commonly Used by Old Age Homes
- Medical Treatment Consent Form
- Home Exercise Program Worksheet
- Forms Used for Mental Health Assessment
- Forms Used by Psychologists
- Medical Forms Commonly Used by/for Students
- Assessment Consent Form
- Forms Used by an Anesthesiologist
- Not Fit to Fly Certificate Template