A nutrition assessment is an elaborate evaluation of patient-related data about dietary intake, lifestyle, and medical history. It is essential to improving food choices, health habits, and living standards. Poor diet and lack of physical activity can result in physical weakness and deranged immunity.
Nutrition
Nutrition is the process of obtaining food necessary for an individual’s growth and health.
There are a few essential elements of nutrition: macronutrients (carbohydrates, fats, proteins, and water) and micronutrients (minerals and vitamins).
Malnutrition refers to food and energy deficiency (undernourishment) and an excess of nutrients (overnutrition). Both should be considered, as their effects may lead to an unbalanced life. Malnutrition is harmful physically and deeply affects a person’s social, personal, and mental health. Its importance is especially vital for children, as it shapes their lives.

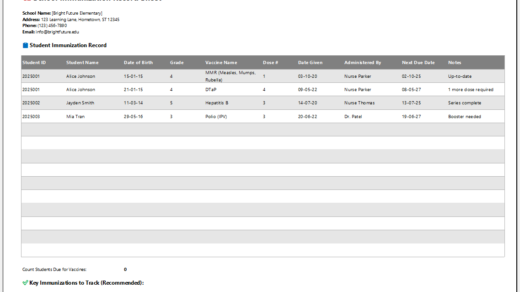
Excel Sheet -[.xlsx Format]
Essentials of Patient Nutrition Assessment
A patient nutrition assessment comprises ABCDs: anthropometric measurements (mentioned ahead), biochemical (laboratory tests), clinical (history and physical examination), and dietary data (to determine whether the patient is malnourished or well-nourished).
Patient Nutrition Assessment Form
The patient nutrition assessment form consists of the following parameters:
- Patient’s name, father’s name, age, sex, blood group, mailing address, phone number, email ID, marital status, employment, religion, race, children, if any with ages, the status of pregnancy, if any, and information about the primary care provider.
- Anthropometric measurements: height, measured weight, ideal weight, waist circumference, basal mass index (BMI), head circumference, mid-upper arm circumference (MUAC).
- History of previous or current illnesses, if any. Duration of illness.
- Information about sports or health goals.
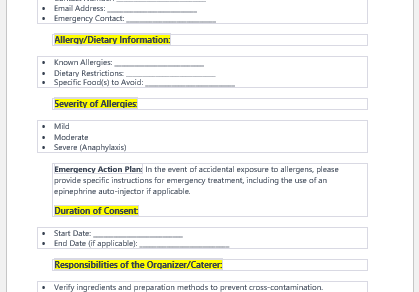
- Treatment, over-the-counter drugs, or supplementation history. Smoking or alcohol abuse with quantification. Allergies and food dislikes, if any.
- The previous record of a physical checkup. All laboratory investigations and radiological tests are recorded.
- Family medical history and any hereditary diseases.
- Activity level: Sedentary (no exercise, gardening, or household work), Moderately active (exercise 3 to 5 times a week, 20 to 30 minutes each time), Active (exercise 3 to 5 times a week, 60 minutes each time), Very active (exercise 3 to 5 times a week, 90 minutes each time), Extremely active (exercise 5 or more times a week, more than 90 minutes each time)
- List of all exercises done by the patient
- Hours spent on different activities, such as watching TV, using a computer, hobbies and recreational activities, the frequency of vacations or trips, and reading or studying.
- Dietary habits include food, meals (breakfast, lunch, dinner, and snacks), and beverages (water, tea, coffee, and juices). Eating patterns and eating disorders, if any.
- Quantifying stress (minimal, considerable, average, unbearable).
- Causes of stress (health-related, job-related, financial, marriage-related, family-related, interpersonal, or spiritual).
- Sleep patterns.
- Undertaking by the patient.
- Privacy and confidentiality agreement.
- Name and signature of the consenter.
- Nursing Documentation Templates
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Pain Diary Worksheet Template
- Forms Commonly Used by Old Age Homes
- Medical Treatment Consent Form
- Home Exercise Program Worksheet
- Forms Used for Mental Health Assessment
- Forms Used by Psychologists
- Medical Forms Commonly Used by/for Students
- Assessment Consent Form
- Forms Used by an Anesthesiologist
- Not Fit to Fly Certificate Template
- Home Visit Consent Form for Schools
- Important Forms Commonly Used by Pharmacies
- Important Forms Commonly Used by Dentists