School-going children need to stay healthy so that there are fewer absentees from school. If a child stays sick and suffers from one thing or another, this results in increased absence from school and ultimately poor performance by the student.
So, a regular checkup and physician’s report are required to know the health status and especially the immunization status of the student. If there is any necessary immunization, it can be picked up by the examination report, and further management can be planned.
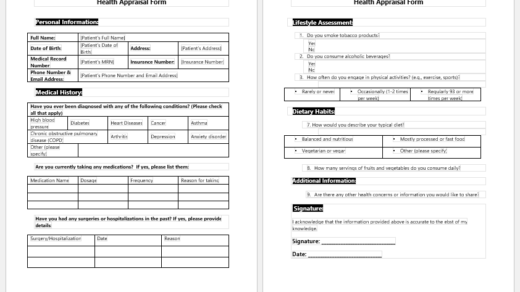
Data Required in Physician’s Report
- The first thing is the identity of the student. His name, age, gender, and the name of the school where he studies are mentioned for identity.
- The name and section of his class, his date of birth, and his complete address with his contact number are also mentioned properly.
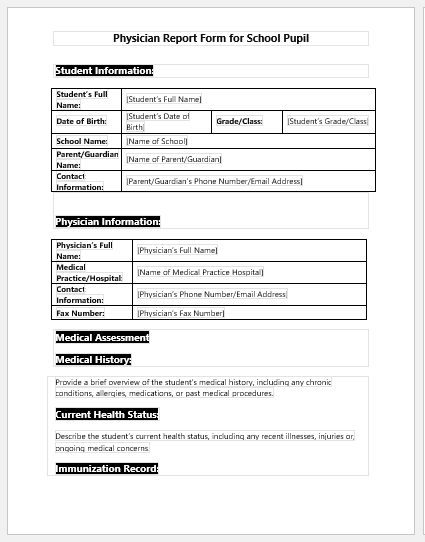
Form Sample
No. of pages = 3
Immunization history of pupil
- The immunization status of the student is very important because children of school-going age are very prone to catch serious infections and if they are not vaccinated or booster doses are not given, there are high chances that they catch and then transfer serious infectious diseases to their schoolfellows. So, the examining physician has to inquire about and mention correctly the vaccination of the student.
- Important diseases against which vaccination is very important are tetanus, pertussis, hepatitis B, polio, tuberculosis, varicella, etc.
- If any student is not vaccinated or vaccination is not recommended, for example, in cases of allergies, a reason is mentioned for this.
- At the end of the vaccination table, we are given two reasons for exemption from vaccination. We have to select which reason is applicable.
Tuberculin Test
- The tuberculin test is the screening test for tuberculosis and is done in all the suspects of T.B. If the student’s history supports that he is likely to have tuberculosis or he has been previously exposed to or suffered from T.B., he must undergo the tuberculin test.
- The doctor has to mention which arm was used for the test and the results of the test by mentioning the diameter of the induration formed.
- If the tuberculin test is positive, the doctor must mention the follow-up plan or suggest anti-tuberculosis therapy.
Medical History
- After the vaccination history and tuberculin test, the medical history of the student is inquired about, and significant points are noted down in the examination form.
- The physician has to mention if the student has any known allergies, asthma, or cardiac or respiratory disorders. Similarly, any other drug, blood transfusion history, skin disorder, or epilepsy history is mentioned with details if identified.
Report of Physical Examination
- In this portion, the physician measures height, weight, vitals, hearing, vision, dental health, and lymph nodes, and all the systemic examination is done.
- Any positive or significant finding is mentioned in detail and further management or suggestions are written in front of each.
- At the end of the examination, the physician signs the report, making it official with his name, contact number, email address, and postal address for follow-up or further reference when required.
- Nursing Documentation Templates
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Pain Diary Worksheet Template
- Forms Commonly Used by Old Age Homes
- Medical Treatment Consent Form
- Home Exercise Program Worksheet
- Forms Used for Mental Health Assessment
- Forms Used by Psychologists
- Medical Forms Commonly Used by/for Students
- Assessment Consent Form
- Forms Used by an Anesthesiologist
- Not Fit to Fly Certificate Template